Managing medical billing for complex medical procedures and diagnoses can be a daunting task. In today’s ever-evolving healthcare landscape, medical facilities and practitioners face numerous challenges related to billing and reimbursement. This article explores effective strategies for handling the complexities of medical billing, ensuring accurate reimbursement, and maintaining financial stability in the face of intricate medical procedures and diagnoses.
Understanding the Complexity
Complex medical procedures and diagnoses often involve a multitude of codes, compliance regulations, and insurance requirements. Medical professionals must accurately document every aspect of the treatment process, including procedures performed, medications administered, and diagnoses made. Any oversight or error in this documentation can lead to claim denials or delays in reimbursement.
1.Stay Updated with Coding and Compliance
Medical coding is the backbone of accurate billing. Regular updates and training for coders and healthcare staff are essential to keep up with changes in medical coding systems (such as ICD-10, CPT, and HCPCS). Compliance with healthcare regulations, including the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA), is crucial to avoid penalties and ensure ethical billing practices.
Importance of Staying Updated:
Accuracy in Billing: Regular updates ensure that medical codes accurately reflect the complexity of procedures and diagnoses. Precise coding is crucial for proper reimbursement and prevents underbilling or overbilling.
Compliance with Regulations: Compliance with regulations such as HIPAA and ACA is mandatory. Staying updated helps healthcare providers adhere to legal requirements, ensuring patient privacy and data security.
Avoiding Penalties: Non-compliance can result in hefty penalties. Keeping abreast of changing regulations helps healthcare facilities avoid legal consequences and financial losses.
Efficient Reimbursement: Proper coding and compliance lead to efficient claims processing. Clean claims are more likely to be processed swiftly, ensuring timely reimbursement.
Strategies to Stay Updated:
Continuous Education: Invest in ongoing training for staff, including coders and healthcare providers. Workshops, webinars, and seminars can provide insights into the latest coding changes and compliance requirements.
Utilize Online Resources: Numerous online platforms offer updates, webinars, and forums where professionals discuss coding challenges and share insights. Subscribing to newsletters and online communities keeps professionals informed.
Collaborate with Industry Experts: Collaborate with coding and compliance experts or organizations. Regular consultations can help healthcare facilities align their practices with the latest industry standards.
Regular Audits: Conduct regular internal audits to identify areas of improvement. Addressing discrepancies promptly ensures that coding and compliance processes are continually refined.
Certifications: Encourage staff to pursue certifications related to medical coding and compliance. Certified professionals are required to stay updated to maintain their credentials, ensuring a knowledgeable workforce.
2.Thorough Documentation
Comprehensive and detailed documentation of medical procedures and diagnoses is fundamental. Encourage healthcare providers to maintain precise records, including the necessity of the procedure, its complexity, and any complications faced. Thorough documentation not only supports accurate billing but also provides a basis for appealing denied claims, if necessary.
Why Thorough Documentation Matters:
Accurate Billing: Detailed documentation provides a clear and comprehensive account of the services rendered, enabling accurate coding. Precise codes are pivotal for claims to be processed correctly, ensuring appropriate reimbursement for complex procedures and diagnoses.
Supports Medical Necessity: Thorough documentation substantiates the medical necessity of a procedure. It outlines the rationale behind the treatment, aiding in justifying the need for complex procedures. This is especially crucial when dealing with insurance pre-authorization and claim disputes.
Facilitates Continuity of Care: Comprehensive records provide valuable insights for fellow healthcare providers, ensuring continuity of care. This is particularly important when patients undergo a series of complex procedures or are diagnosed with intricate medical conditions. Clear documentation aids in seamless information transfer between healthcare professionals.
Legal Compliance: Adequate documentation ensures compliance with legal regulations, including those outlined in the Health Insurance Portability and Accountability Act (HIPAA). It safeguards patient privacy and confidentiality while allowing authorized personnel access to necessary medical information.
Supports Resedevelop new treatments, and enhance overall healthcare practices. Documented information plays a vital role in advancing medical science.
Best Practices for Thorough Documentation:
Be Specific and Detailed: Document all aspects of the patient encounter, including symptoms, diagnoses, treatment plans, procedures performed, and medications prescribed. Include date and time stamps for each entry.
Use Standardized Terminology: Ensure consistency by using standardized medical terminology. This helps in clear communication and understanding among healthcare professionals and coders.
Record Changes and Updates: Document any changes in the patient’s condition, treatment plans, or prescribed medications. Timely updates provide an accurate reflection of the patient’s healthcare journey.
Include Justifications: Clearly state the medical necessity of procedures and treatments. Explain why a specific procedure was chosen and how it contributes to the patient’s overall healthcare.
Collaborate with Care Team: Encourage collaboration among healthcare providers. Ensure that specialists, nurses, and other staff members document relevant information to create a comprehensive patient record.
Use Electronic Health Records (EHR): Implementing EHR systems streamlines documentation processes. EHRs provide structured templates, reduce errors, and facilitate secure information sharing among authorized healthcare professionals.
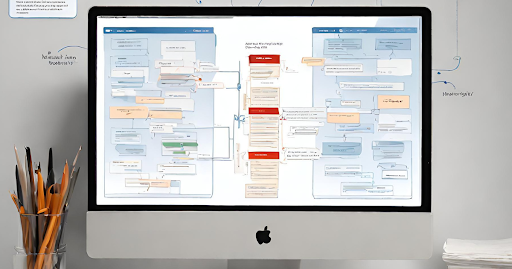
3.Implement Technology Solutions
Leveraging advanced medical billing software and electronic health record (EHR) systems can streamline the billing process. These technologies can automate coding, submission, and tracking of claims. Automated systems reduce the likelihood of human errors, improve efficiency, and accelerate the reimbursement cycle.Here’s how embracing technology can revolutionize medical billing practices in the face of intricate medical cases:
Automation and Efficiency:
a. Billing Software: Implementing specialized medical billing software automates mundane tasks such as data entry, coding, and claims submissions. These systems are equipped with advanced algorithms that ensure accurate code selection, reducing the risk of human errors. Automation accelerates the billing cycle, leading to faster reimbursements.
b. Electronic Health Records (EHR): Integration of EHR systems centralizes patient information, including medical history, diagnoses, and treatment plans. This integration ensures that billing is based on real-time, accurate data, reducing discrepancies and denials. EHRs also facilitate seamless communication among healthcare providers, ensuring comprehensive and cohesive patient care.
Coding Accuracy and Compliance:
a. AI-Powered Coding Assistants: Artificial intelligence (AI) tools analyze medical records to suggest appropriate codes based on the documented procedures and diagnoses. These AI-powered assistants enhance coding accuracy, ensuring that the complexity of procedures is correctly represented, leading to accurate reimbursement.
b. Compliance Checkers: Technology solutions can incorporate compliance checkers that continuously monitor billing practices against the latest regulations. Automated alerts notify staff of potential compliance issues, allowing for proactive resolution and preventing costly penalties due to non-compliance.
Enhanced Communication and Transparency:
a. Patient Portals: Patient portals enable transparent communication regarding billing matters. Patients can access their billing information, understand charges, and receive electronic statements. Clear communication fosters trust and minimizes disputes, ensuring a positive patient experience.
b. Secure Messaging Systems: Implementing secure messaging systems within EHR platforms allows healthcare providers to communicate internally, ensuring that billing-related queries are promptly addressed. This enhances collaboration among administrative staff, coders, and healthcare professionals, leading to more accurate billing practices.
Data Analytics for Revenue Optimization:
a. Predictive Analytics: Advanced data analytics tools can predict revenue patterns, identify billing trends, and foresee potential issues. By analyzing historical data, healthcare facilities can optimize their billing strategies, anticipate cash flow fluctuations, and proactively address challenges.
b. Performance Dashboards: Interactive dashboards provide real-time insights into billing performance metrics. Key performance indicators (KPIs) such as claim acceptance rates, denial rates, and average reimbursement times are visually represented. Monitoring these metrics empowers healthcare administrators to make data-driven decisions, enhancing overall revenue management.
4.Verify Insurance Coverage

Before performing a complex medical procedure, verify the patient’s insurance coverage thoroughly. Understand the terms and conditions of the insurance policy, including pre-authorization requirements and coverage limitations. Clear communication with patients about their financial responsibilities helps prevent disputes and ensures a smoother billing process. Here’s why verifying insurance coverage is so critical and how healthcare professionals can approach this process effectively:
Avoid Claim Denials:
a. Pre-Authorization Requirements: Many complex medical procedures necessitate pre-authorization from insurance providers. Verifying these requirements beforehand ensures that the procedure is approved, preventing claim denials due to lack of pre-authorization.
b. Understanding Policy Limitations: Different insurance policies come with varying coverage limitations. Verifying these limitations, such as maximum allowable amounts for specific procedures or the number of allowed visits, prevents overbilling and denials, ensuring claims are processed smoothly.
Prevent Financial Disputes:
a. Clear Communication: Verifying insurance coverage enables clear communication with patients regarding their financial responsibilities. Patients need to understand their co-pays, deductibles, and any out-of-pocket expenses. Transparent communication prevents financial disputes, fostering trust and satisfaction.
b. Coverage Exclusions: Certain procedures or treatments might be excluded from coverage under specific policies. Verifying coverage helps healthcare providers inform patients about potential out-of-pocket expenses, avoiding surprises and disputes after the procedure.
Streamline Billing Processes:
a. Accurate Billing Information: Verifying insurance coverage ensures accurate patient information, policy numbers, and coverage details are recorded. This accurate data is vital for submitting clean claims, reducing the likelihood of errors or rejections.
b. Timely Claim Submissions: With verified insurance information, claims can be submitted promptly after the procedure. Timely submissions increase the chances of swift processing and reimbursement, ensuring a healthy cash flow for healthcare providers.
Strategies for Effective Verification:
a. Dedicated Verification Team: Assign a dedicated team or staff member responsible for insurance verification. Having a specialized team ensures consistency and accuracy in the verification process.
b. Utilize Technology: Insurance verification software and tools automate the verification process. These tools can cross-verify patient information with insurance databases, providing real-time, accurate results.
c. Document Verification Details: Maintain detailed records of the verification process, including the date and time of verification, the staff member responsible, and the information obtained. This documentation serves as a reference in case of disputes or discrepancies.
d. Regular Training: Regularly train staff involved in the verification process. Ensure they are well-versed in understanding insurance policies, including complex clauses and limitations, enabling them to verify coverage effectively.
5.Train Staff Effectively

Proper training for administrative and medical staff is pivotal. Staff should be educated about the nuances of billing for complex procedures and diagnoses. Regular training sessions and workshops can enhance medical procedures and their understanding of coding updates, compliance regulations, and the importance of accurate documentation. Here’s why staff training is crucial and how healthcare facilities can approach it effectively:
Keep Up with Industry Changes:
a. Regular Updates: Medical billing codes, regulations, and procedures are constantly evolving. Regular training programs keep staff updated with the latest industry changes, ensuring that billing practices align with current standards.
b. Specialized Workshops: Conduct specialized workshops focusing on complex procedures and diagnoses. These workshops delve into specific coding challenges and compliance issues, equipping staff with in-depth knowledge.
Enhance Coding Proficiency:
a. Specialized Training Modules: Develop training modules focusing on intricate coding systems such as ICD-10, CPT, and HCPCS. In-depth training ensures staff members understand the nuances of coding for complex medical cases.
b. Mock Scenarios: Create mock scenarios mimicking real-life complex cases. Staff members can practice coding and documentation in a controlled environment, refining their skills before encountering similar cases in actual practice.
Foster Effective Communication:
a. Interdepartmental Collaboration: Encourage collaboration between billing, administrative, and medical staff. Effective communication ensures that billing staff can clarify any uncertainties directly with medical professionals, reducing errors and improving accuracy.
b. Patient Communication Skills: Train staff in effective patient communication, especially regarding financial matters. Staff should be able to explain complex billing details to patients in a clear, empathetic, and understandable manner, reducing confusion and enhancing patient satisfaction.
Compliance Training:
a. HIPAA Compliance: Conduct regular HIPAA compliance training to ensure staff members understand patient privacy laws and regulations. This knowledge is vital to safeguard patient information and maintain legal compliance.
b. Ethical Billing Practices: Instill the importance of ethical billing practices. Staff members should be aware of regulations related to upcoding, unbundling, and other fraudulent billing activities, emphasizing the facility’s commitment to integrity.
Utilize Online Resources:
a. Online Courses: Encourage staff to enroll in online courses and webinars. These resources often offer flexibility and cover a wide range of topics, allowing staff to enhance their skills at their own pace.
b. Coding Communities: Join coding communities and forums where staff members can discuss challenges, share insights, and learn from the experiences of peers. Active participation fosters continuous learning and problem-solving skills.
Regular Assessments and Feedback:
a. Knowledge Assessments: Conduct regular knowledge assessments to gauge staff proficiency. Identify areas where additional training is needed and tailor future training programs accordingly.
b. Feedback Loops: Create feedback mechanisms where staff can provide input on training programs. Staff insights are valuable in shaping future training initiatives and ensuring they meet the specific needs of the team.
6. Outsource Billing Services

Consider outsourcing medical billing to specialized companies or professionals. Outsourcing allows healthcare providers to focus on patient care while experts handle the complexities of billing. These professionals are well-versed in the latest coding practices, compliance regulations, and insurance protocols, ensuring accurate and timely reimbursement.Here’s why outsourcing medical billing services is advantageous and how healthcare providers can approach this option effectively:
Expertise and Specialization:
a. Industry Proficiency: Outsourced billing services providers specialize in medical billing. Their teams are well-versed in the complexities of coding, compliance regulations, and insurance protocols, ensuring accurate and efficient billing processes for complex medical cases.
b. Continuous Training: Outsourcing companies invest in continuous training for their staff, ensuring that they stay updated with the latest coding practices, compliance regulations, and industry advancements. This expertise translates into accurate billing and minimizes claim denials.
Cost-Efficiency:
a. Reduced Overheads: Outsourcing eliminates the need for in-house billing staff, reducing overhead costs associated with salaries, benefits, and training programs. This cost-efficiency contributes to overall savings for healthcare facilities.
b. Scalability: Outsourced billing services can scale according to the healthcare facility’s needs. Whether handling a few complex cases or managing the billing for an entire hospital, outsourcing providers can adjust their services accordingly, ensuring flexibility and cost-effectiveness.
Increased Focus on Patient Care:
a. Time and Resources: Outsourcing medical billing frees up valuable time and resources for healthcare providers. With billing responsibilities off their plate, healthcare professionals can concentrate entirely on patient care, enhancing the quality of services provided.
b. Patient Satisfaction: Enhanced focus on patient care leads to improved patient satisfaction. When healthcare providers can dedicate their time to patients instead of administrative tasks, it fosters positive patient-provider relationships.
Technology Integration:
a. Advanced Software: Outsourcing companies often use advanced billing software and electronic health record (EHR) systems. These technologies streamline the billing process, reduce errors, and improve efficiency. Healthcare providers benefit from the latest tools without having to invest in expensive software themselves.
b. Data Security: Reputable outsourcing companies employ state-of-the-art data security measures, ensuring the confidentiality and integrity of patient information. This protects healthcare facilities from potential data breaches and legal consequences.
Focus on Core Competencies:
a. Core Operations: Medical facilities can focus on their core competencies, such as patient diagnosis and treatment, without being burdened by the complexities of billing. Outsourcing allows healthcare providers to concentrate on what they do best while billing experts handle the financial aspects.
b. Strategic Growth: With streamlined operations and reduced administrative burdens, healthcare facilities can strategically plan for growth, invest in new technologies, and expand their services, ultimately benefiting both the facility and its patients.
Conclusion:
Managing medical billing for complex procedures and diagnoses demands a strategic approach, continuous education, and the integration of technology. By staying updated with coding practices, ensuring thorough documentation, implementing technology solutions, verifying insurance coverage, training staff effectively, and considering outsourcing options, medical facilities and practitioners can navigate the complexities of medical billing successfully. Adopting these strategies not only enhances revenue streams but also fosters a transparent and efficient billing process, ultimately improving patient satisfaction and the overall healthcare experience.
Recent Comments