Revenue Cycle Management (RCM) emerges as a critical player in the healthcare ecosystem, ensuring the seamless flow of finances and supporting the sustainability of medical practices. In this article, we delve into the importance of Revenue Cycle Management in medical billing, shedding light on its impact on healthcare organizations and the overall quality of patient care.
Understanding Revenue Cycle Management
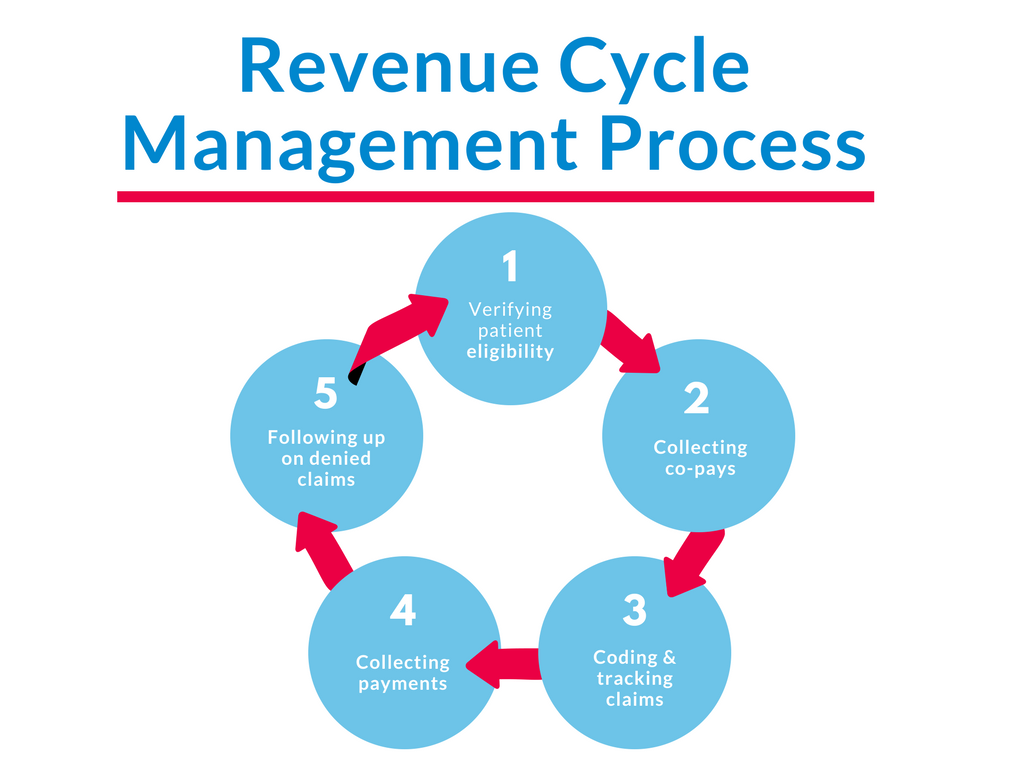
At its core, Revenue Cycle Management refers to the process of managing the financial aspects of a patient’s journey through the healthcare system, from appointment scheduling to the final payment of a bill. It encompasses a series of interconnected steps, including patient registration, insurance verification, coding, billing, and ultimately, reimbursement.
1. Enhancing Financial Stability
The effective implementation of Revenue Cycle Management significantly contributes to the financial stability of healthcare organizations. By streamlining billing processes and reducing claim denials, RCM ensures a steady and predictable cash flow, allowing medical facilities to allocate resources efficiently and invest in advanced technologies for improved patient care.
Let’s delve deeper into how RCM enhances the financial well-being of medical practices:
Streamlined Billing Processes:
Efficient RCM systems streamline the entire billing process, from the initial patient encounter to the submission of claims and receipt of payments. By automating repetitive tasks, such as data entry and claims processing, RCM minimizes delays and reduces the likelihood of billing errors. This streamlined approach ensures that medical bills are processed swiftly, contributing to a consistent and predictable cash flow.
Reduced Claim Denials:
Unresolved or denied claims can significantly impact a healthcare organization’s revenue stream. RCM employs sophisticated software and predictive analytics to validate claims before submission, minimizing the chances of denials. This proactive approach not only accelerates the reimbursement process but also decreases the administrative burden associated with claim resubmissions.
Optimized Revenue Capture:
Comprehensive RCM systems ensure that healthcare providers capture the full revenue to which they are entitled. Through accurate coding, thorough documentation, and diligent charge capture processes, RCM helps prevent underbilling or missed opportunities for reimbursement. This optimization is crucial for maximizing revenue potential and maintaining financial health.
Effective Accounts Receivable Management:
Timely and efficient management of accounts receivable is essential for financial stability. RCM tools monitor and manage outstanding payments, facilitating prompt follow-ups on unpaid claims. By minimizing the time it takes to collect payments, healthcare organizations can enhance liquidity and reduce the risk of bad debt.
Cost Reduction Through Automation:
The automation of routine and time-consuming tasks in the revenue cycle not only improves accuracy but also reduces operational costs. By minimizing manual intervention, RCM allows healthcare organizations to allocate resources more efficiently, directing them toward patient care, staff development, and technological advancements that contribute to overall financial sustainability.
2. Reducing Billing Errors by implementation of Effective Revenue Cycle Management:

Accuracy is paramount in medical billing, and RCM plays a pivotal role in minimizing errors. Automated coding systems and thorough documentation help prevent billing discrepancies, ensuring that healthcare providers receive fair compensation for the services rendered. This not only benefits the healthcare organization but also promotes transparency in financial transactions, enhancing trust between patients and providers.
Automated Coding Systems:
RCM systems often incorporate advanced automated coding tools that help ensure accurate coding of medical procedures and diagnoses. Automation reduces the likelihood of manual errors, such as incorrect code selection, which can lead to claim denials and delayed payments. These systems leverage sophisticated algorithms to enhance coding precision and compliance with industry standards.
Thorough Documentation:
Comprehensive documentation is the backbone of accurate medical billing. RCM emphasizes the importance of thorough and detailed documentation of patient encounters, treatments, and procedures. By standardizing documentation processes and maintaining a complete and accurate medical record, RCM minimizes errors related to missing or incomplete information, ultimately improving the accuracy of billing.
Regular Staff Training:
Keeping healthcare staff well-trained and updated on coding and billing regulations is essential. RCM systems often include training modules that enable staff to stay informed about changes in coding guidelines, compliance requirements, and industry best practices. Regular training sessions contribute to a knowledgeable and skilled workforce, reducing the probability of billing errors.
Real-time Claim Scrubbing:
Many RCM solutions offer real-time claim scrubbing capabilities. This involves a thorough review of claims for errors or missing information before submission. By identifying issues at the point of data entry, RCM helps prevent common errors such as duplicate billing, inaccurate patient information, or coding discrepancies, resulting in cleaner claims and faster reimbursement.
3. Optimizing Staff Efficiency:
Implementing an effective RCM system reduces the administrative burden on healthcare staff. Automation of routine tasks, such as claims processing and billing inquiries, allows medical professionals to focus on their primary role—delivering quality patient care. This optimization of staff efficiency contributes to a more productive and satisfied workforce.

Automation of Routine Tasks:
RCM systems automate repetitive and time-consuming tasks associated with billing processes. This includes tasks such as data entry, claim submission, and payment posting. By automating these routine activities, healthcare staff can redirect their time and efforts toward more critical responsibilities, such as patient care and complex problem-solving.
Integration with Electronic Health Records (EHR):
Seamless integration between RCM and Electronic Health Records (EHR) eliminates the need for duplicate data entry. Staff members can access patient information and billing details from a centralized system, reducing the risk of errors and saving time previously spent toggling between different platforms.
Streamlined Appointment Scheduling:
RCM systems often include features that streamline appointment scheduling processes. Efficient scheduling tools help staff manage patient appointments more effectively, reducing wait times, minimizing scheduling conflicts, and optimizing the use of available resources. This contributes to a smoother patient flow and enhances overall staff efficiency.
Reduced Manual Claim Verification:
RCM systems incorporate automated verification processes for insurance information, reducing the need for manual verification by staff. Automated verification ensures that accurate and up-to-date insurance details are used for billing purposes, minimizing errors and saving time that would otherwise be spent on manual checks.
4. Improving Patient Experience:
A seamless and transparent billing process positively impacts the overall patient experience. By providing clear and concise information about costs, insurance coverage, and payment options, healthcare organizations foster trust and satisfaction among patients. A positive experience extends beyond the clinical setting, influencing patient loyalty and the reputation of the medical practice.
Transparent Financial Communication:
RCM emphasizes clear and transparent communication regarding financial matters. Patients appreciate receiving accurate and understandable information about their healthcare costs, insurance coverage, and expected out-of-pocket expenses. Transparent communication helps build trust and ensures that patients are well-informed about the financial aspects of their care.
Patient-friendly Billing Processes:
RCM aims to simplify and streamline the billing process. Patient-friendly billing statements, easy-to-understand invoices, and clear explanations of charges contribute to a positive experience. By presenting information in a user-friendly format, RCM helps alleviate confusion and reduces the stress associated with navigating complex billing documents.
Efficient Insurance Verification:
RCM systems automate insurance verification processes, ensuring that patients receive accurate information about their coverage. This efficiency minimizes delays in processing claims and helps patients understand their financial responsibilities upfront. Quick and precise insurance verification contributes to a smoother overall patient experience.
Flexible Payment Options:
RCM supports the implementation of flexible payment options for patients. By providing choices such as online payment portals, installment plans, or automatic payment setups, healthcare organizations make it easier for patients to manage their financial obligations. This flexibility enhances patient satisfaction and fosters a positive perception of the billing process.
5. Compliance and Risk Mitigation:
The healthcare industry is subject to a complex web of regulations, and compliance is non-negotiable. Revenue Cycle Management systems are designed to navigate this regulatory landscape, reducing the risk of legal complications and penalties. By staying up-to-date with industry standards, RCM ensures that healthcare organizations operate within legal boundaries.
Adherence to Regulatory Standards:
RCM systems are designed to stay abreast of ever-changing healthcare regulations. They incorporate features that help healthcare organizations adhere to industry standards, billing codes, and compliance requirements. By automating processes in accordance with these standards, RCM minimizes the risk of regulatory violations.
Real-time Compliance Audits:
RCM platforms often include real-time compliance auditing features. These tools continuously monitor billing practices, coding accuracy, and documentation completeness. By identifying potential compliance issues promptly, healthcare organizations can address them proactively, reducing the risk of audits, fines, or legal actions.
Documentation Integrity:
Accurate and thorough documentation is critical for compliance. RCM emphasizes the importance of maintaining comprehensive and compliant records. By automating documentation processes and implementing standardized protocols, RCM minimizes the risk of incomplete or inaccurate documentation that could lead to compliance issues.
Fraud Detection and Prevention:
RCM systems incorporate algorithms and analytics to detect anomalies that may indicate fraudulent activities. By analyzing patterns in billing data, RCM helps identify potential instances of fraud or abuse. This proactive approach aids in preventing fraudulent activities before they escalate, protecting the organization from legal and financial repercussions.
Recent Comments