Medical billing is a critical aspect of the healthcare industry, ensuring that healthcare providers receive timely and accurate compensation for the services they render. In this complex landscape, the term “clean claim” holds immense significance. Understanding what a clean claim is and how it affects the billing process is essential for healthcare professionals, administrators, and patients alike. We will explore the concept of clean claims in medical billing and its importance.

What Is a Clean Claim?
A clean claim is a medical billing term that refers to a healthcare insurance claim that is submitted correctly and accurately the first time, requiring no additional information or corrections for processing. It contains all the necessary information and documentation needed for prompt and efficient processing, reducing the likelihood of claim denials, delays, or disputes. Clean claims contribute to the smooth operation of the healthcare reimbursement system.
Key Elements of a Clean Claim
To be considered a clean claim, a medical insurance claim must meet specific criteria, which include:
- Complete and Accurate Information: A clean claim contains all the necessary patient information, provider details, diagnosis and procedure codes, insurance policy details, and itemized service charges. Any missing or incorrect information can lead to claim rejection.
- Timely Submission: Claims should be submitted within the insurance company’s designated time frame to ensure that they are processed promptly. Delays in submission can lead to claim denials.
- Proper Documentation: Supporting documentation, such as medical records, must be attached if required by the insurance company. This documentation should substantiate the medical necessity of the services rendered.
- Compliance with Billing Guidelines: Claims must adhere to the specific billing and coding guidelines of the insurance company. This includes using accurate Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes.
Importance of Clean Claims
Clean claims play a crucial role in the healthcare billing process for various stakeholders, including healthcare providers, insurance companies, and patients. Here’s why they are important:
- Faster Reimbursement: Clean claims are processed swiftly, leading to faster reimbursement for healthcare providers. This helps maintain their cash flow and reduces financial strain.
- Lower Administrative Costs: Healthcare providers save time and money by submitting clean claims, as they reduce the need for administrative work to correct errors and resubmit claims.
- Enhanced Patient Satisfaction: Quick and accurate claims processing results in timely billing and lower out-of-pocket expenses for patients, improving their overall satisfaction.
- Efficient Workflow: Clean claims contribute to the efficiency of healthcare facilities by minimizing claim rejections and disputes. This allows healthcare staff to focus on patient care rather than administrative tasks.
- Reduced Claim Denials: Clean claims are less likely to be denied or rejected by insurance companies, reducing the need for appeals and resubmissions.
The Benefits of Clean Claims
Here are some key benefits of clean claims:
Expedited Reimbursement
One of the most significant advantages of clean claims is that they are processed more rapidly by insurance companies. Since all the required information is complete and accurate, there is no need for additional back-and-forth communication between the provider and the payer. This means healthcare providers receive their payments more quickly, ensuring a healthier cash flow for their organizations.
Reduced Denials and Rejections
Clean claims have a significantly lower chance of being denied or rejected by insurance companies. Common reasons for claim denials include missing or incorrect information, coding errors, and insufficient documentation. By submitting clean claims, healthcare providers can minimize these issues, resulting in less time and effort spent on claim resubmissions and appeals.
Enhanced Efficiency
Efficiency is crucial in the healthcare industry. Clean claims allow billing staff to focus on processing new claims, resolving complex issues, and improving the overall revenue cycle. This improved efficiency benefits both the healthcare provider and the insurance company, as it reduces administrative overhead and costs.
Improved Cash Flow
Clean claims lead to more predictable and consistent revenue streams. When claims are processed without delays or rejections, healthcare providers can better plan their budgets, invest in technology and staff, and ultimately provide a higher quality of care to their patients. A consistent cash flow is essential for the financial stability of any healthcare organization.
Enhanced Reputation
Timely, accurate claims processing positively impacts the reputation of healthcare providers. Patients appreciate it when their claims are handled efficiently, and they are more likely to remain loyal to providers who consistently offer a hassle-free billing experience. In the long run, this can lead to increased patient retention and referrals.
Regulatory Compliance
Clean claims are more likely to be in compliance with healthcare regulations and payer policies. This reduces the risk of audits, fines, and legal issues, which can be detrimental to a healthcare organization’s finances and reputation.
Cost Savings
By reducing the number of denied or rejected claims and streamlining the billing process, healthcare providers can save on administrative costs. The time and resources saved can be redirected toward patient care and other important aspects of the business.
The Role of Medical Billing Companies in Ensuring Clean Claims

- Accurate Data Entry and Coding: Medical billing companies play a key role in precise data entry and coding. Each medical action needs specific codes like CPT and ICD to categorize and bill claims properly. Errors in coding can lead to denied claims or payment delays. Skilled coders at these companies make sure the codes match the services, reducing the risk of claim rejection.
- Verification of Patient Information: Clean claims require accurate patient info. Billing companies confirm patient details like demographics and insurance coverage to avoid claim denials. Checking and updating patient information is crucial to send clean claims to insurers.
- Compliance with Regulations:
- Healthcare rules change a lot, and medical billing companies keep track of these changes. They make sure claims follow the latest rules, reducing the risk of rejection due to non-compliance. This knowledge is crucial for getting claims accepted.
- Claims Scrubbing and Error Prevention:
- Before sending claims to insurers, billing companies use software and experts to find and fix errors. This cuts down on claim rejections by spotting missing info, duplicates, and other problems. This proactive approach helps get clean claims and faster payments.
- Timely Submission: Quickly sending claims is crucial for efficiency. Billing companies make sure claims are sent on time to avoid payment delays. Timely submission also keeps cash flow steady for healthcare providers.
- Denial Management: If a claim is denied, billing companies are skilled at managing it. They figure out why it was denied, appeal if needed, and resend corrected claims quickly. This helps reduce the financial hit from denials and makes sure providers get their reimbursement.
The Profound Effects of Clean Claims on Healthcare Practices

In the ever-evolving landscape of healthcare, providers face numerous challenges that can impact their financial stability and operational efficiency. Many often overlook one critical aspect of healthcare management, which has a substantial impact: submitting clean claims. Clean claims are accurate, complete, and error-free submissions to insurance companies. In this article, we will explore the far-reaching effects of clean claims on healthcare practices, highlighting the benefits of accurate claims submission and ways to optimize the process.
- Accelerating Reimbursement: Clean claims speed up reimbursement by containing all necessary info, reducing denials and communication. This boosts cash flow and financial stability for healthcare practices.
- Reducing Denials and Appeals: Clean claims reduce denial risk, saving time and money for healthcare practices. Denied claims are costly and resource-intensive to resolve, making clean claims a valuable focus.
- Enhancing Revenue Integrity: Clean claims guarantee full reimbursement for healthcare services, maintaining financial viability by preventing underpayments or non-payments. Accuracy and completeness are essential for revenue integrity.
- Improved Patient Satisfaction: Clean claims ensure accurate and timely billing, boosting patient satisfaction and trust. Happy patients are more likely to return and refer others, vital for any healthcare practice.
- Streamlined Workflow: Smooth claims processing starts with a simple process. When we always send clean claims, the work to manage claims becomes easier. This makes things better for the people doing paperwork, and it lets healthcare providers focus on taking care of patients instead of dealing with claims problems.
- Compliance and Risk Mitigation: Clean claims keep healthcare practices in line with rules, avoiding legal and money problems. Billing mistakes can lead to audits, fines, and legal trouble. By putting clean claims first, providers can lower these risks and stay on the right side of the law.
Optimizing the Effects of Clean Claims
Now that we’ve established the profound effects of clean claims on healthcare practices, let’s discuss strategies for optimizing the process:
- Staff Training: Invest in training and continuous education for your billing and coding staff to ensure they are up-to-date with industry standards and regulations.
- Electronic Health Records (EHR) Systems: Implement an EHR system that integrates billing and coding processes, reducing the likelihood of data entry errors.
- Regular Auditing: Conduct regular internal audits to identify and correct issues in the claims submission process before they become problematic.
- Outsourcing: Consider outsourcing billing and coding to professional firms with expertise in clean claims submission.
- Clear Communication: Encourage open communication between billing, coding, and clinical staff to resolve issues and discrepancies promptly.
- Technology Integration: Invest in technology solutions that facilitate clean claims submission, such as software that automatically checks claims for errors.
Easy Steps to Ensure a Clean Claim: Streamlining Your Healthcare Billing Process
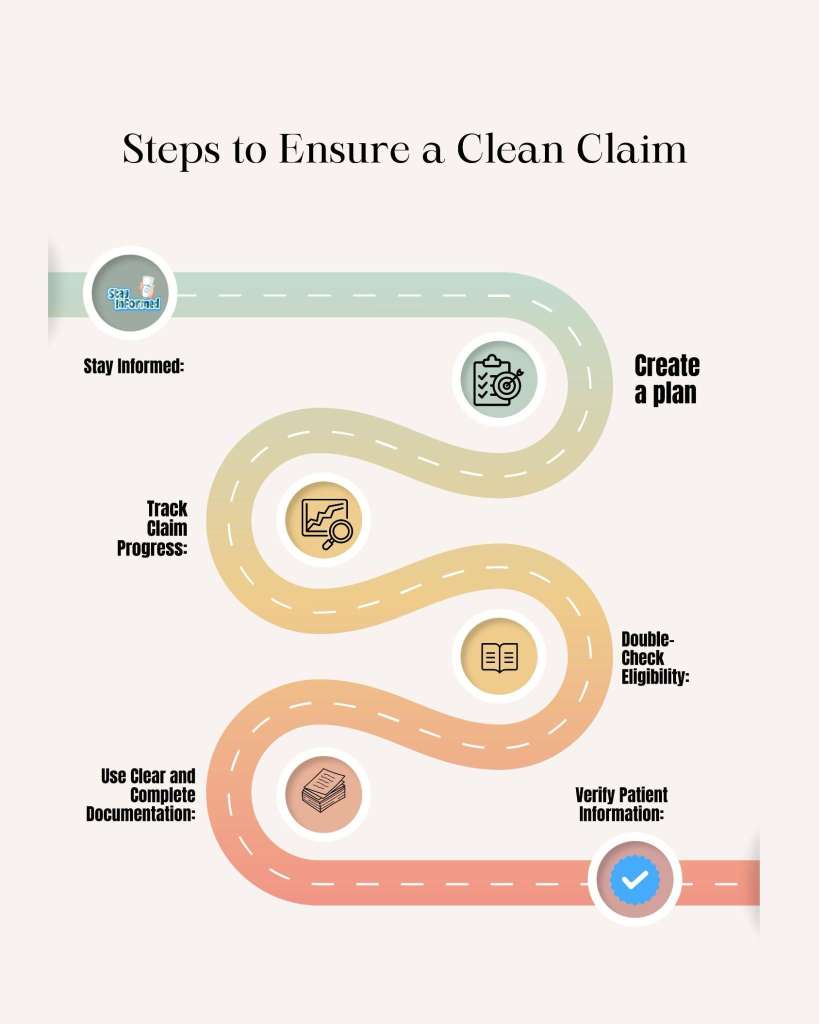
By following a few easy steps, you can streamline your billing process and ensure that your claims are clean, reducing the chances of delays or denials. Let’s explore these steps to make your healthcare billing more efficient.
Verify Patient Information
The first crucial step in ensuring a clean claim is to verify and update patient information. Ensure that all personal details, insurance information, and contact information are up-to-date and accurate. This reduces the chances of claim rejection due to incorrect information.
Use Clear and Complete Documentation
Medical coding relies heavily on the information documented in patient charts. Ensure that your documentation is clear, legible, and complete. This is essential for accurate coding and billing. Invest in electronic health records (EHR) systems that can streamline and improve documentation.
Double-Check Eligibility
Before submitting a claim, verify the patient’s insurance eligibility. Ensure that the patient’s coverage is active and that the services are covered under their plan. This reduces the likelihood of claim denials due to insurance issues.
Track Claim Progress
Establish a system to track the progress of your claims. This can help identify any potential issues early on and allow you to take corrective action. Many billing software programs offer tracking features.
Stay Informed
Healthcare billing and coding are constantly evolving. Stay informed about changes in regulations, coding updates, and billing requirements to ensure that your claims are compliant with the latest standards.
Conclusion
In the intricate world of medical billing, understanding what constitutes a clean claim is essential. It ensures that healthcare providers receive timely and accurate reimbursement for their services, streamlining the revenue cycle. Healthcare professionals, administrators, and patients should collaborate to ensure that they submit claims correctly the first time, benefiting all parties involved. By adhering to the key elements of a clean claim and staying informed about billing guidelines, healthcare providers can optimize their billing processes and maintain a healthy financial outlook.
.
Recent Comments